Empowering Nurses Through Education.
With help from a study guide & practice review question book bundle, PNW classes, and online education by Nicole Kupchik.
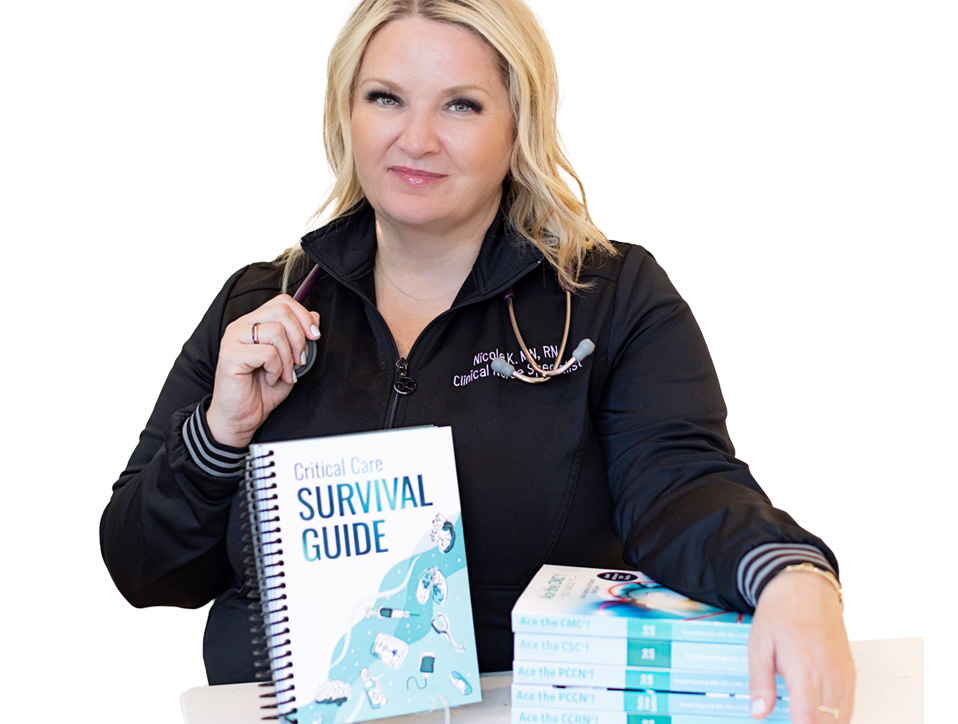
Nicole Kupchik, MN, RN, CCNS, CCRN-CMC, PCCN, has been a Critical Care RN for over 25 years. She uses her knowledge and expertise to arm nurses around the country with tools to create safe work and practice environments.
Her casual style sets the tone for a relaxed, fun & interactive learning environment. Find out how Nicole can help you.
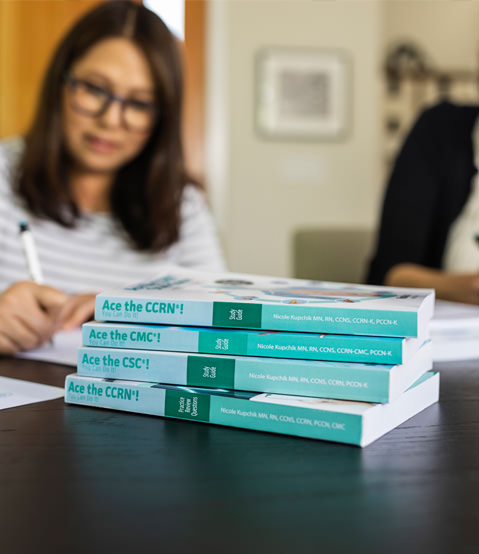
Ace Your CCRN®, PCCN®, CMC® or CSC® Certification Exams!
Interested? Learn More